Sideroblastic Anemia
Learn about the causes, symptoms, diagnosis and lab findings of sideroblastic anemia
PATHOLOGY
4/5/20252 min read
Sideroblastic anemia is a rare but intriguing condition where the bone marrow produces ringed sideroblasts instead of healthy red blood cells (erythrocytes). These immature red cells accumulate iron in their mitochondria, failing to properly form hemoglobin, the molecule responsible for carrying oxygen throughout the body. Let’s delve into its causes, symptoms, diagnosis, and treatment in a clear, engaging, and informative way.
What is Sideroblastic Anemia?
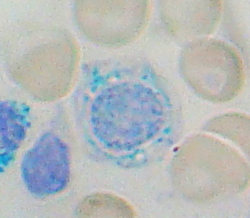
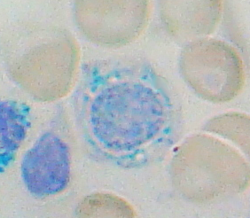
At its core, sideroblastic anemia disrupts red blood cell production, leading to oxygen transport inefficiencies. The name comes from the hallmark feature—ring sideroblasts—immature red blood cell precursors that show a striking accumulation of iron in their mitochondria. These iron-loaded cells, highlighted using a Prussian blue stain, create a ring-like appearance, a defining characteristic of this condition.
This unusual process happens because of defective heme synthesis. Heme, an essential part of hemoglobin, requires iron to bind with protoporphyrin, but when this binding fails, iron builds up in the mitochondria.
Why Does This Condition Occur?
The root cause of sideroblastic anemia lies in the interruption of the biochemical pathway required for heme production. Key culprits include:
Protoporphyrin Deficiency: Without this molecule, iron cannot integrate into heme.
Genetic Mutations: Inherited defects like X-linked sideroblastic anemia can hinder critical enzymes, such as δ-ALA synthase.
Secondary Factors: Environmental or external triggers, such as:
Alcohol Use: A mitochondrial toxin that impacts cell functions.
Vitamin B6 Deficiency: Often caused by medications like isoniazid, disrupting δ-ALA synthase activity.
Lead Poisoning: Potentially interfering with heme synthesis enzymes.
Symptoms of Sideroblastic Anemia
The symptoms of this condition can range from subtle to severe, often linked to anemia and iron overload:
Common Anemia Signs:
Fatigue, weakness, and pallor (pale skin).
Shortness of breath, headaches, and dizziness.
Heart palpitations due to low oxygen delivery.
Iron Overload Issues:
Joint pain and skin darkening (bronzing).
Endocrine disturbances like diabetes from iron deposits in organs.
Advanced Cases: Potential enlargement of the spleen or liver due to chronic anemia.
How is Sideroblastic Anemia Diagnosed?
Effective diagnosis of sideroblastic anemia involves meticulous laboratory and clinical evaluations:
Blood Tests: Show microcytic, hypochromic anemia (small, pale red blood cells).
Iron Studies:
Increased Serum Iron and Ferritin: Indicating iron overload.
Decreased TIBC (Total Iron Binding Capacity): Reflecting reduced capacity to bind excess iron.
Bone Marrow Examination:
Highlights the presence of ring sideroblasts using Prussian blue staining.
Erythrocyte Protoporphyrin Levels: Reduced levels confirm impaired heme synthesis.
Genetic Testing: Useful for identifying hereditary cases like X-linked sideroblastic anemia.
Treatment Options for Sideroblastic Anemia
Treatment aims to address the underlying cause, correct anemia, and manage iron overload. Here's how:
General Treatments:
Vitamin B6 (Pyridoxine) Therapy: Often effective for hereditary forms caused by δ-ALA synthase deficiency.
Iron Chelation Therapy: Medications like deferoxamine help remove excess iron from the body.
Secondary Cause Management:
Stopping alcohol consumption and discontinuing harmful medications.
Treating lead poisoning through chelation therapy.
Blood Transfusions: Sometimes necessary for severe anemia, but they may exacerbate iron overload.
Bone Marrow Transplantation: Considered in rare, severe hereditary cases unresponsive to other treatments.
Key Takeaways
Sideroblastic anemia is a complex yet fascinating condition. While its causes range from genetic mutations to environmental triggers, understanding its cellular mechanisms helps demystify its effects on red blood cell production and iron metabolism. With early diagnosis and tailored treatments, patients can manage their condition effectively and lead fulfilling lives.
